If you or a loved one has sustained a bedsore in a RI or MA Nursing home, you may be entitled to compensation for medical bills, pain and suffering and other losses. Our law firm works with experienced nursing home bedsore lawyers in RI and MA and there is no fee until you get a settlement or award. Please contact us toll free or online for a free (no obligation) consultation.

Have You Seen Evidence of Your Loved One Developing a Bedsore While in a Nursing Home?
Call Today for a Free Case Evaluation!
How Do Bedsores Develop?
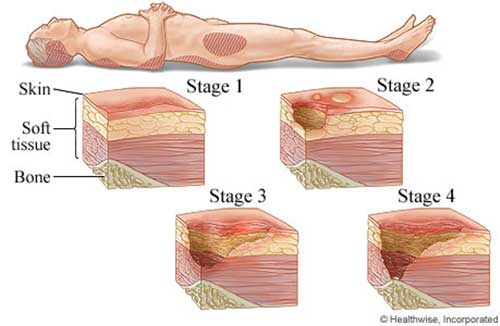
Individuals who cannot easily move around can develop pressure ulcers, also known as bedsores. These sores are caused by continued pressure against the skin that limits blood flow and circulation. The tissue beneath the skin becomes damaged and then begins to break down. Oftentimes, the affected area will become red or inflamed. After the breakdown of the skin, open sores begin to develop. In severe cases, the sores can cause destruction of muscle and even bone.
Bedsores (sometimes called “decubitus ulcers” or “dermal ulcers”) often occur in patients who are confined to wheelchairs or lay in bed for long periods of time. Other risk factors include poor nutrition, persistent wetness, and other chronic medical issues such a peripheral artery disease. The most important factor in preventing bedsores is to avoid long-term pressure on one part of the body. In patients with limited mobility, this requires routine position changes.
How Can Bedsores Be Prevented?
In order to prevent bed sores, it is important to assess the patient’s risk factors and develop a plan to prevent pressure sores as soon as possible. Medical professionals commonly use a method known as the Braden Scale to predict a patient’s likelihood of developing pressure sores. The Braden Scale evaluates several risk factors including the patient’s activity level, ability to sense discomfort, diet, and ability to move. Another large factor is the patient’s ability to control their bladder and bowels. After this assessment, nursing home employees should coordinate a plan that will incorporate regular movement and routine toileting and bathing to prevent sores.
Routine skin checks can reveal the formation of bedsores. While giving care, nursing home staff should check the patient’s skin to make sure no ulcers are forming. Certain areas of the body, such as the back, shoulders, buttocks, hips, and heels are more prone to pressure sores and should be checked more often in higher risk patients.
How Can Nursing Homes Be Responsible For Bedsores?

The formation of bedsores and pressure sores can often be an indication of abuse or neglect. Nursing homes may be responsible for the formation of bedsores if they fail to properly assess a patient’s risk level, if they do not change the patient’s position regularly, or do not properly toilet and bathe the patient. Also, nursing home staff may cause a bedsore to get much worse if they do not treat the patient promptly and properly after the sore is diagnosed.
What are Common Signs and Symptoms of Bedsores?

Bedsores and pressure sores often develop quickly and appear in stages ranging from mild to severe. The first stage usually results in redness or inflammation around the site of the sore. The next stage occurs when a break in the skin develops exposing the soft tissue below the skin. If the sore is not treated promptly at this stage, the sore will worsen and the surrounding tissue and skin will continue to break down. The most serious stage of a bedsore occurs when muscle and bone are damaged and sometimes even visible. Sometimes, skin or damaged tissue can become stuck to the patient’s bed or lead to a serious infection. Common signs and symptoms of pressure sores include the following:
- Changes in skin color or texture
- Swelling or puffiness
- Redness or inflammation
- Pus-like drainage from affected area
- Skin that feels cool or warm to touch
- New area of tenderness or pain
- Painful skin lesions that smell bad
- Open wounds or breakage of skin
What You Should I Do If My Loved One Develops Bedsores?
If your loved one develops a bedsore:
- Make sure your loved one is receiving appropriate wound care for the existing bedsore.
- If your loved one cannot easily move on her own, ensure she is receiving appropriate care, including regular repositioning and support, to prevent future bedsores.
- If you suspect nursing home neglect or abuse, consult with an experienced nursing home bedsore lawyer.
Why Should You Call d’Oliveira & Associates?

If you or a loved one have been injured while receiving care at an assisted living, elder care, or nursing home facility, then you should consider talking to lawyer about your legal options. The experienced Rhode Island nursing home bedsore lawyers that we work with can file a lawsuit on your behalf and charge no fee unless you win an award or settlement. Contact us toll-free at 1-800-992-6878, or submit an online contact form for a free (no obligation) case evaluation.
Sources:
